In an eggshell...
- Polycystic Ovary Syndrome, or PCOS, is a hormonal condition that affects women in their reproductive years.
- It can mess with your periods, throw in some extra male hormones, and even sneak in these tiny cysts on your ovaries.
- It might make getting pregnant or undergoing fertility treatments a bit tricky due to the diverse symptoms
At its base, PCOS is a hormonal disorder, affecting 4-10% of women worldwide.
Hormones are the messengers in our body, the signals for which are secreted by the brain 🧠.
They tell the organs how much of and when to release specific hormones.
And when the gears for this system, especially for female hormones get a little rusty, it can result in several symptoms.
And for PCOS this looks like- irregular periods, acne, weight gain, and excessive hair growth to name a few.
And with a diagnosis like this, comes a ton of questions around PCOS, how it affects us, our fertility and more.
So we reached out to doctors, embryologists and experts to compile this guide on PCOS, for you to refer to!
Let’s dive in!
What is PCOS?
Polycystic Ovarian Syndrome (PCOS) is a condition where the ovaries produce excess hormones. This leads to an overall hormonal imbalance in the body.
Let’s do a breakdown of what it means:
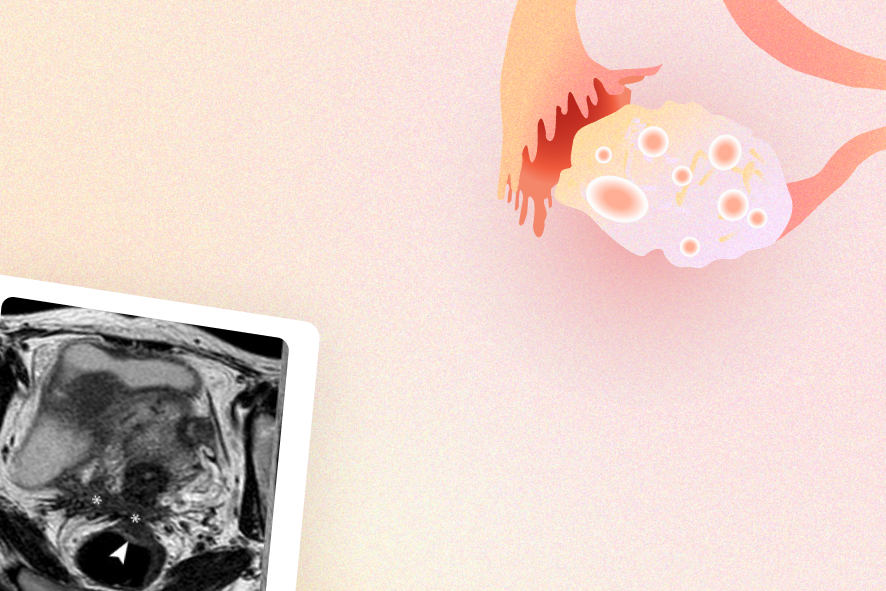
Poly refers to ‘many’
Cyst refers to an abnormal sac that contains fluid.
Ovaries are the female reproductive organs which contain follicles and eggs, and produce hormones.
And syndrome is a set of medical signs and symptoms that occur together.
Is PCO and PCOS the same?
Actually, no. Polycystic Ovary Syndrome (PCOS) and Polycystic Ovaries (PCO) are related but distinct issues.
When doing an ultrasound, a doctor may use the term ‘PCO’ to describe the appearance of the ovaries having more follicles than usual. This occurs due to an imbalance in hormones but for a short period of time.
The TLDR? Your body can regulate back, and it doesn't necessarily mean you have PCOS.
On the other hand, doctors may use the term ‘PCOS’ to describe the appearance of the ovaries having more follicles than usual. This is also due to an imbalance in hormones but it lasts for longer periods, harder for the body to regulate alone.
The TLDR? Due to the combination of specific symptoms and their length, this is classified as PCOS.
🥸Nerd it out: Download our free PCOS guide
What are the symptoms of PCOS?
Now, as we mentioned above, PCOS affects more than just our menstrual cycles. PCOS has to do with the endocrine system. The major signs of PCOS boil down to three key symptoms:
- Enlarged ovaries that contain multiple cysts, seen via ultrasound scans
- Irregular periods or no ovulation
- Hormonal imbalances such as elevated androgen levels and insulin resistance
According to the Rotterdam criteria, if two or three of these factors are present, then a PCOS diagnosis may be likely.
Additionally, other symptoms include:
- Acne
- Weight gain
- Excess hair growth
- Thinning hair
- Darkening of the skin
- Headaches
- Mood changes
- Inflammation of the gut
Here’s a breakdown of why exactly these symptoms occur:
Insulin resistance
As per stats, 65-70% of people with PCOS suffer from insulin resistance, especially those who are overweight, but it can also affect lean women.
Insulin resistance is when the body no longer responds to signals from the hormone, insulin. This leads to high blood sugar levels. As a result, sugar cannot enter body cells and isn't used by the body.
But why does it happen?
The food we eat is our body’s source of energy. Food gets broken down into molecules, most of which are sugar molecules, also called glucose.
Since cells need this to function, our pancreas produce insulin, basically the vehicle that transports glucose around and balances the sugar levels in your blood.
Sometimes, the routine gets disrupted and your body falls into a cycle called ‘insulin resistance.
In this case, cells may have too much glucose already and don't want more. They become resistant to insulin and sugar stays in the blood, causing both insulin and blood sugar levels to rise, causing a sequence of negative effects on the reproductive system.
Excess androgens
Hyperandrogenism is a condition where androgens, (such as testosterone) are excessively produced. It occurs in 60-80% of PCOS-affected individuals and is also a risk factor.
Excess androgens tend to affect our menstrual cycles by affecting the number of follicles recruited every month. Excess follicles growing can lead to some developing to cysts, or not releasing an egg at all.
It can also cause androgenic alopecia, which is permanent hair loss in some regions of the scalp causing baldness. It also causes hirsutism which is increased hair growth, particularly in areas such as the face, chest, or back
Lastly, it can also cause dark patches in the skin, especially in areas such as around the neck, groin and under breasts, along with acne due to increased sebum (oil) production in the skin.
Irregular or no ovulation
Women with PCOS may face issues in their menstrual cycle such as irregular ovulation, secondary amenorrhea (periods that stop for three or four months in a row) or abnormal uterine bleeding.
This is due to hormonal imbalances in the body, leading to subfertility or infertility. This is due to the lack of ovulation or regular periods which can make detecting your fertile window harder, thus making it harder to conceive.
Causes of Polycystic Ovary Syndrome
With PCOS, there is no exact cause, but rather a combination of factors.
PCOS also shows up differently due to a blend of genetic predisposition and external factors.
Let’s look into a breakdown of the causes:
Epigenetic Factors
These could be irregularities in our genes passed down via generations, or even factors such as nutrition or environment. For example, stress is also considered an epigenetic factor.
Chronic stress can lead to changes in gene expression and hormonal balance, potentially impacting the development and severity of PCOS.
Environmental factors
Diet, stress, activity level, and lifestyle may also influence the onset of PCOS.
Endocrine factors
Hormonal imbalance ends up impacting other hormones, follicle development, egg maturation, and fertility.
How is PCOS diagnosed?
Here’s the catch: a diagnosis is not always straightforward.
The severity and symptoms of PCOS can vary among people. For example, some women may exhibit all three symptoms and have a clear diagnosis of PCOS.
On the other hand, some may experience one symptom very faintly, leading to a misdiagnosis.
That’s why, given the range of symptoms, a diagnosis can happen at any stage. Here’s how different practitioners might identify PCOS:
- Dermatologists: may give PCOS as a cause if you suffer from hair loss, thinning of the hair, darkened patches on the body, or acne
- Dieticians: if you are finding it difficult to lose weight or are gaining weight quickly, especially if you have a family history of heart disease or type 2 diabetes.
- General practitioners: may review your medical history and symptoms, and conduct a physical exam by looking for signs such as acne, increased body weight, and excessive hair growth (hirsutism). They may order blood tests for hormone levels and request an ultrasound scan for you.
- Gynaecologists: This is where a diagnosis is most common and likely. Gynaecologists may do pelvic ultrasounds where multiple follicles may be detected. They can also recommend hormonal blood tests such as AMH to check for abnormal levels.
PCOS risk factors
While we cannot pinpoint a single cause, research does suggest some risk factors that can increase your chances of getting PCOS, such as:
- A family history of PCOS
- Obesity
- Insulin resistance
- A non-active lifestyle
- Stress
Treatment of PCOS
Whilst there’s no exact cure for PCOS, there are lots of treatment options that can help with the symptoms.
Managing weight
For instance, reducing between 5-10% of overall body weight or having a BMI between 18.5 and 24.9 can significantly improve symptoms and reduce long-term effects.
Regular exercise
With regular exercise, you promote a healthy metabolism, which indirectly supports liver function and helps the body manage toxins. It also balances mood and reduces stress levels, benefiting PCOS symptoms.
Avoid insulin spikes
Eating small, frequent meals throughout the day helps keep your blood sugar steady. Choose foods that don’t cause big sugar spikes, and always include some protein and fibre
It’s also essential to not starve yourself before you eat, which helps reduce the rise of cortisol levels (a stress hormone produced by the adrenal glands).
Managing stress
Stress can contribute greatly to PCOS. Our work, environment or just intensive periods of stress in our lives can make our body become accustomed to the heightened state of stress, which can affect our hormonal balance.
To regulate this, you can experiment with different methods such as working on trauma and building more self-love, journaling and even joining communities of women with PCOS.
Lifestyle changes
Having a diet rich in natural, unprocessed food, with lean meat, antioxidants, fruits, vegetables and so on can also add a layer of benefit.
Medications
If you face irregular or absent periods, the oral contraceptive pill or birth control pills may be recommended to induce regular periods. These have a combination of oestrogen and progesterone which decrease androgen production and regulate oestrogen.
You may also be recommended Metformin, which is known as an insulin sensitising drug, is usually used in the treatment of type 2 diabetes but helps control blood sugar levels.
Supplements
Supplementing may help regulate bone health and metabolic function. We also suggest working with a doctor or alternative doctor to understand your individual needs as they would know the best combination of supplements for you.
Where Amilis comes in
Battling PCOS is hard on its own.
And especially if you want to opt for fertility treatments such as egg freezing, you may find yourself with a baggage of questions.
So, we’re here to answer: Is egg freezing possible with PCOS?
Yes, and in fact, we at Amilis are working to help thousands of women in the UK navigate this question.
From the first step of “what tests should I even do” to “which clinic should I go ahead with?”, Amilis comes in and helps you every step of the way, via:
- Discounted prices on fertility tests, such as AMH and full hormone panel (at price is 50% cheaper than fertility clinics)
- Get free consultations with expert doctors across the UK
- Free consultations with vetted fertility clinics near you
And if you’re still looking to take the first step, get started with our fertility quiz.
It’s about time we make fertility care accessible, not a luxury.
And we’re paving the way for it, one day at a time 🙌🏼



.png)


.png)


