Contents
- Overview of egg freezing medication
- How many days of injections does egg freezing include?
- Egg freezing protocols for cancer patients
- Where do I purchase egg freezing medication?
- How to store and use egg freezing medication
- Where do I inject egg freezing medication?
- Side effects of egg freezing medication
- What is the cost of egg freezing medication
- How Amilis can help
- Frequently asked questions
In an eggshell...
- Egg-freezing injections are hormones that help grow your follicles and eggs for retrieval
- These are medications that help grow follicles, prevent ovulation and help mature the eggs before egg retrieval
- On average, total medication costs typically range from £500 to £2500 per cycle
“You’ll need these injections, here’s how to apply them, make sure they’re at the right time, and you’d have to come in for scans too”
If you’re someone who’s been through egg freezing you would’ve heard this. If not, this is something you might hear, if you opt for the procedure.
Egg-freezing injections are hormones that are injected in a planned manner to grow your follicles and eggs for retrieval.
And no, it’s not just about following a timeline and making sure you inject the medications.
It’s about how you feel emotionally, helping you plan for the timeline, how you may experience some side effects, tips on where to inject these meds, and how to go about finishing your medication cycle.
So at Amilis, we decided to curate this guide on egg-freezing medication. It’s about what type of hormones are used, what to expect, tips to inject, cost considerations and more!
Ready? Let’s dive in!
Overview of egg-freezing medication
We can break down the medication process into 2 main stages:
Pretreatment
These include:
- Oral contraceptive pills or birth control pills to trigger ovulation in women with irregular or absent cycles. This also reduces the chances of cysts and helps time the egg-freezing cycle
- Prenatal vitamins or supplements such as CoQ10, folic acid, selenium, and vitamin D may be prescribed before the cycle
- Medications such as HgH (Human Growth Hormone) which may help promote the growth of follicles
Treatment protocols
🧫To grow the follicles
These are the primary medications used in egg-freezing cycles. They help release gonadotropins, hormones that stimulate the ovaries to produce multiple follicles.
🥸 Let's nerd it out here for a second: these injections trigger the brain to release FSH and LH, to grow follicles, and thus eggs. Below are some of the medications you may be prescribed during your cycle:
- Gonal-F (follitropin alfa): This is a recombinant form of FSH, and it's created in a laboratory to closely mimic the body's natural FSH. It's typically administered as a subcutaneous injection once daily.
- Menopur (menotropins): This medication contains both FSH and LH. It's derived from the urine of post-menopausal women and is also given as a daily subcutaneous injection. The addition of LH can be beneficial for some women, particularly those over 35 or with diminished ovarian reserve.
- Follistim (follitropin beta): Another recombinant FSH option, similar to Gonal-F.
The dosage of these medications is carefully calibrated based on factors such as your age, AMH levels, antral follicle count, and body mass index. Your healthcare provider will monitor your response through blood tests and ultrasounds, adjusting the dose as needed.
🥚To stop egg release
Again, a mini “nerd it out” 🥸. Naturally, egg release happens in our body due to a surge in the LH hormone, followed by a smaller surge of FSH.
Medications such as GnRH antagonists and agonists prevent premature ovulation or egg release. They do this by blocking the body's natural LH surge. These are suggested along with the medications for follicle growth.
- Cetrotide (cetrorelix acetate): Usually started around day 5-6 of stimulation. This is given as a daily subcutaneous injection until the trigger shot.
- Ganirelix (ganirelix acetate): Like Cetrotide, it's another option for preventing premature ovulation.
These medications ensure that the developing eggs remain in the ovaries until they're mature enough for retrieval.
💉Trigger medication
The trigger shot initiates the final maturation of the eggs and sets ovulation in motion.
Hey, but didn’t we just say we don’t want ovulation happening?
Yeah, natural ovulation. If the eggs leave the ovary, we won’t be able to retrieve them.
So, we time when we want the eggs to be ready, using these medications, bypassing our body’s natural signals. The trigger medication is also more for the maturation part and ensuring that the eggs are ready.
It's typically given during the final stages of your medication cycle around 34-36 hours before the scheduled egg retrieval.
- hCG (Pregnyl, Ovitrelle): This mimics the natural LH surge. It's very effective but carries a higher risk of OHSS in some patients. While this is the most common trigger, in cases where there is a higher risk of OHSS, an alternate trigger may be provided.
- Lupron (leuprolide acetate): A GnRH agonist that causes a surge of both FSH and LH. It's often used to prevent OHSS in high-risk patients.
- Kisspeptin: Kisspeptin is a newer option that stimulates a more natural hormone surge. It can help reduce OHSS risk while maintaining good egg maturation rates.
Some protocols may use a combination of these triggers, known as a dual stimulation cycle. This is to optimise results and minimise risks.
How many days of injections does egg freezing include?
On average, the entire stimulation process takes about 11-14 days or 2-3 weeks. It starts from the day you get your period and begin medications.
Based on your egg-freezing protocol, around 11-14 days of hormone injections are needed. For instance, here’s how a sample egg-freezing protocol might look like:
Day 1-5: Gonal F+ Menopur
Day 6-8: Gonal F+ Menopur+ Ganirelix
Day 9: Gonal F+ Menopur+ Ganirelix+ HcG trigger (if dual trigger, HcG+ Lupron)
Day 10: No medication
Day 11: Egg retrieval
In this sample protocol, Gonal F and Menopur stimulate follicles and eggs. Ganirelix prevents natural ovulation, and the HcG triggers ovulation at the right time before retrieval.
Egg freezing protocols for chemotherapy/ cancer patients
For patients with cancer, egg or embryo freezing is a recommended procedure before starting chemotherapy. In such cases, there are two things to take into consideration:
- how much time they have until chemotherapy
- And whether the cancer is oestrogen sensitive (grows in the presence of oestrogen).
Based on this, common stimulation protocols for egg freezing cannot be used. This is because they have stimulation with Gonadotropin-releasing hormone (aka the hormone that tells the pituitary gland to release FSH), which also results in the release of oestrogen.
Hence, the protocols are modified to include:
- Letrozole + FSH
- Tamoxifen + FSH
This combination helps recruit more follicles, develop and retrieve mature eggs. The bonus? All with a decreased amount of FSH compared to conventional protocols.
There were also some studies that mentioned a lower egg yield from letrozole cycles. But given that it’s the safest method out there so far, the study justified its usage and proposed having two consecutive cycles safely, in case of less egg yield.
Where do I purchase egg-freezing medication?
Once you’ve been given the go-ahead for your cycle, the next step is to purchase the egg-freezing medication. Here's a more detailed look at the process:
1. Prescription: Your fertility clinic will provide a prescription for the medications. This will include details on the specific drugs, dosages, and instructions for use.
2. Specialty Pharmacies: Most egg-freezing medications are only available through speciality pharmacies that focus on fertility treatments. Your clinic may have an in-house pharmacy or partnerships with specific pharmacies and can provide recommendations.
3. Ordering Process: Once you have your prescription, you'll need to contact the pharmacy to place your order. Many speciality pharmacies offer online ordering and home delivery.
4. Insurance Coverage: Check with your insurance provider about coverage for fertility medications. Some plans may cover part or all of the cost, while others may not cover fertility treatments at all.
How to store and use egg-freezing medication
For starters, It's best to order your medications well in advance of your cycle start date. Aim to have them in hand at least 2-3 days before you're scheduled to begin injections.
Once you receive your medications, check the storage requirements carefully. Some need refrigeration, while others can be kept at room temperature. This is important because proper storage is needed to maintain the medication's efficacy.
Your medication kit may include the medicine in a vial, a prefilled syringe, a needle for mixing and one for injecting, and some alcohol swabs.
Where do I inject egg-freezing medication?
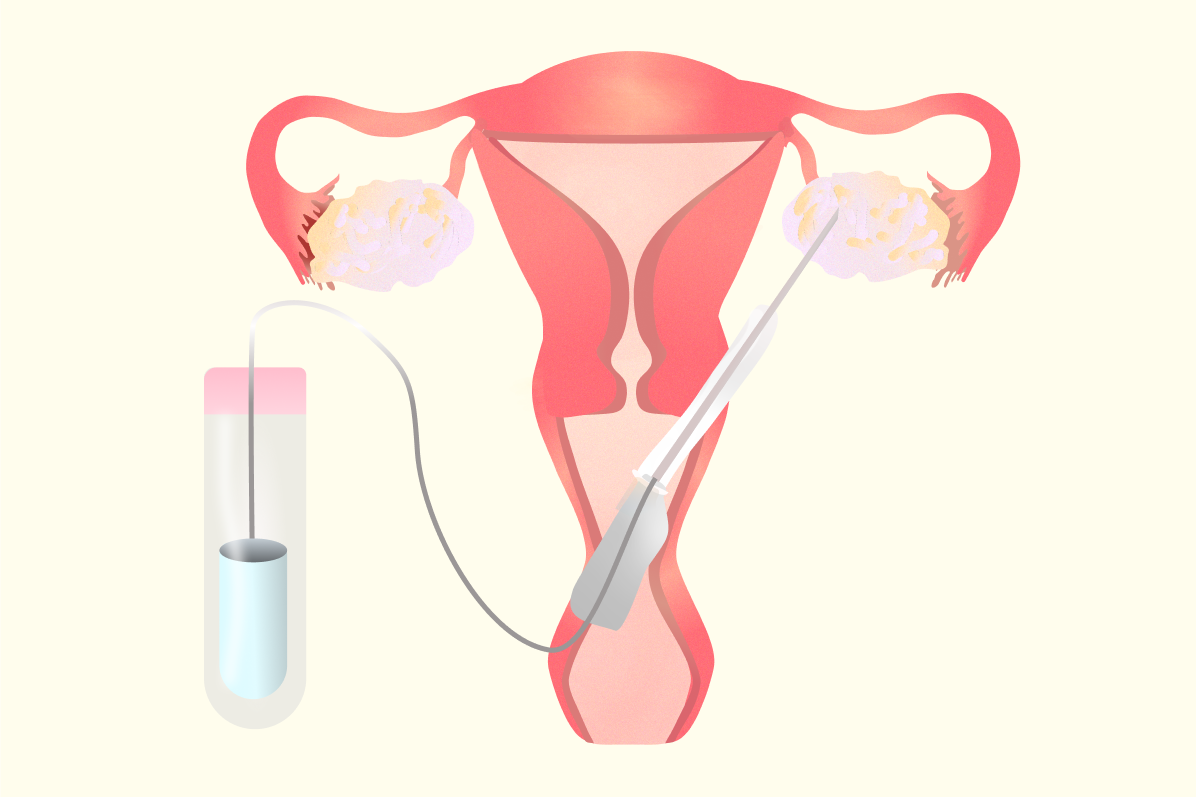
Egg-freezing medication can be injected in two ways.
- The first one is intramuscular, given into the muscle and is less common
- The second one is subcutaneous which is more common and is given under the skin.
For follicle growth shots and medications that stop egg release, subcutaneous is the common route. It’s usually done in the lower stomach, an inch below or to the side of the belly button. It’s advised to pinch your skin before injecting as it helps.
Trigger medications are usually intramuscular, and can be administered by a nurse or a partner/friend.
Our pre-vetted egg freezing clinics offer injection training resources, and support for any questions or issues that arise with medications during your cycle. These can be incredibly helpful for learning proper injection techniques and administering the medications yourself.
Side effects of egg-freezing medication
Since these are hormonal medications 💊, they tend to carry along their small baggage 🧳 of side effects. While these medications are generally well-tolerated, it's important to be aware of potential side effects. Let's explore these in more detail:
Common egg-freezing hormone side effects:
1. Injection site reactions: Redness, swelling, or bruising at the injection site is common. These are usually mild and resolve quickly.
2. Bloating: As your ovaries enlarge due to follicle growth, you may experience abdominal bloating and discomfort.
3. Breast Tenderness: Hormonal changes due to medication can cause your breasts to feel swollen or sensitive.
4. Mood swings: Hormonal fluctuations may affect your mood, leading to irritability or emotional sensitivity.
5. Headaches: Some women experience headaches, particularly in the first few days of stimulation.
6. Fatigue: The hormonal changes and the stress of the process can lead to feelings of tiredness.
Less common side effects
1. Nausea: Some women may experience mild nausea, especially later in the stimulation process.
2. Pelvic Discomfort: As the ovaries enlarge, you may feel heaviness or mild pain in your pelvic area.
3. Hot Flashes: Particularly with the use of GnRH antagonists, some women experience hot flashes.
4. Allergic Reactions: While rare, some may have allergic reactions to the medications. Always inform your doctor of any known allergies.
Rare side effects
Ovarian Hyperstimulation Syndrome (OHSS)
One such risk that healthcare providers are also on the cautious side for is OHSS. It happens when the ovaries swell up due to the overproduction of eggs in response to the stimulation medications.
And by rare, we mean the chances of it occurring is between 3.1 and 8%.
Symptoms of OHSS can range from mild to severe. Your healthcare provider will make sure to monitor you throughout your cycle for any hormonal indicators of OHSS. This is to prevent it from happening.
For mild cases, symptoms may include severe bloating, abdominal pain, rapid weight gain, nausea and vomiting, decreased urination and shortness of breath.
While mild cases may occur, it’s very rare for severe cases to occur.
📚Also read: Our guide to OHSS and egg-freezing
What is the cost of egg-freezing medication?
On average, total medication costs typically range from £500 to £2500 per cycle. While costs can vary based on individual protocols, here's a general range for patients in the UK:
- Follicle-stimulating injections: £500-£1,500 per cycle
- Ovulation prevention medications: £200-£400 per cycle
- Trigger shot: £50-£150
Different factors can affect the cost of egg freezing, and knowing them beforehand can help with financial planning. Here's a more detailed breakdown:
1. Medication protocol and cycles: The specific combination and dosage of medications, and the number of cycles involved can impact the cost.
2. Duration of stimulation: The stimulation process is usually around 11-14 days. But in case you are prescribed any supplements or OCPs (Oral contraceptive pills) as pre-treatment, it may affect the cost.
3. Individual response: This is based on your monitoring appointments or protocols. You may have higher doses, or an added trigger to have a good response, which may affect the cost.
4. Pharmacy: Prices can vary between pharmacies, sometimes significantly. If you're planning multiple cycles, ask your pharmacy if they offer discounts for bulk purchases.
5. Insurance coverage: Some insurance plans may cover part or all of the medication costs.
Also check: What’s the average cost of egg freezing in London?
How Amilis can help
We get it. Having to go through the consultations, and coming to terms with the fact that there’s an entire timeline of medication can feel like a lot.
But there are resources out there that can help with the process. And our team at Amilis (that’s us 👋) strives to do the same.
Amilis can help with:
- 1-1 consultations with the Amilis team if you’re new and exploring whether this option is right for you
- Affordable fertility tests to help you understand your ovarian reserve
- Free consultations with our partner clinics, reducing costs on your cycle
Or, you could even take our personalised egg-freezing quiz to explore and weigh this option for you.
The bottom line? We’re here to make fertility accessible, affordable and on your terms.
We’ve got you covered❤️
Frequently asked questions
- What are some Menopur alternatives?
Alternatives to Menopur include Meriofert, Pergoveris, Fostimon, Gonal-F, Bemfola, Gonal-F, Follistim, and Bravelle. Your doctor will determine the best option based on your individual needs.
- Does Ganirelix stop follicle growth?
No, Ganirelix doesn't stop follicle growth per se, but it prevents them from releasing eggs too early (premature ovulation) by blocking the natural LH surge. Occasionally when Ganirelix is added (usually mid-cycle) there is a slight levelling out of oestrogen level rise and your doctor may raise the dose of stimulation slightly to counteract this.
- Do follicles grow after Lupron trigger?
-Yes, follicles can continue to grow after any trigger because they have their own granulosa cells inside them, producing hormones and causing expansion of the follicles.
- Are Cetrotide and Ganirelix interchangeable?
-yes, Cetrotide, Ganirelix and Fyremedel are all GnRH antagonists and are interchangeable even within the same stimulation cycle. Your doctor will prescribe the most suitable option for your protocol.
- Does Pregnyl need to be refrigerated?
“HCG (Pregnyl) can be kept at room temperature as a powder. Once it has been reconstituted (mixed with water) it should be kept in the fridge and used within 60 days” says Dr Vivienne. “But if you accidentally leave it out of the fridge don’t worry, it should be ok for 2 or 3 days. However, most patients are instructed to mix the powder and the water the same day as the trigger injection, so the need to keep it refrigerated is not really relevant”.






.png)


